Background. CD5 expression is rare in MZL and has been historically characterized in case series of splenic (SMZL) and nodal (NMZL) MZL (Baseggio et al., haematologica, 2010; Jaso et al., Am J Clin Pathol, 2013; Salido et al., Blood 2010). These studies reported similar outcomes with CD5+ and CD5- MZL but did not examine the significance of CD5 in the context of modern immunochemotherapy. BR is a regimen increasingly used for treatment of MZL, but many patients can initially receive R monotherapy (R-mono) with no detriment to survival (Olszewski et al., ASH 2019). There are no biomarkers predictive of differential response to R-mono or BR. We examined outcomes of these treatments in MZL according to CD5 expression.
Methods. We collected clinicopathologic data on patients with MZL (SMZL, NMZL, and extranodal MZL of the mucosa-associated lymphoid tissue [MALT]) diagnosed in our center between 2010 and 2020. CD5+ MZL was diagnosed by expert academic hematopathologists after excluding chronic lymphocytic leukemia and mantle cell lymphoma by immunophenotypic evaluation and cytogenetic/fluorescent in-situ hybridization studies. For prognostication, we assigned subtype-specific prognostic scores: MALT-IPI (Thieblemont et al., Blood 2017), IIL score for SMZL (Arcaini et al., Blood 2006), and standard IPI for NMZL. We examined overall response rate (ORR), progression-free (PFS) and overall survival (OS), calculated from the start of therapy, according to CD5 expression and first-line therapy. Survival was compared using log-rank tests stratified by age, MZL subtype, and stage.
Results. The study included 213 patients with SMZL (N=51, 24%), NMZL (N=46, 22%), and MALT (N=116, 54%), with median age of 68 years at diagnosis, and with 52% women. Overall, 23 MZLs (10.8%) were CD5+. CD5 expression was most common in SMZL (24%), then NMZL (11%), and rare in MALT lymphoma (5%; P=.003). CD5+ cases showed del(7q) in 9%, trisomy 12 in 17%, and CD23 expression in 9%. All tested CD5+ cases had a positive peripheral blood flow cytometry (100% vs 65% of CD5- cases, P<.001) and bone marrow involvement (100% vs 64%, P=.004). Furthermore, adjusting for variable prevalence in MZL subtypes, CD5 expression was significantly associated with high lactate dehydrogenase (LDH, 56% vs 18%, adjusted odds ratio (aOR) 5.74, P=.0008), anemia (39% vs 20%, aOR 2.55, P=.044), monoclonal paraprotein (75% vs 36%, aOR 5.33, P=.016), advanced stage (83% vs 54%, aOR 4.10, P=.013), and blood involvement (78% vs 32%, aOR 7.80, P=.0001). CD5 expression also correlated with a higher IIL score in SMZL (P=.032 on test for trends of odds), higher IPI in NMZL (OR=2.84, P=.09), and higher MALT-IPI (OR=3.38, P=.10). CD5+ MZL had a numerically higher prevalence of 17p deletion (43% vs 21%, P=.35) and complex karyotype (42% vs 22%, P=.26) than CD5- MZL, when tested. Histologic transformation occurred in 2 (9%) CD5+ and 4 (2%) CD5- MZLs (P=.13).
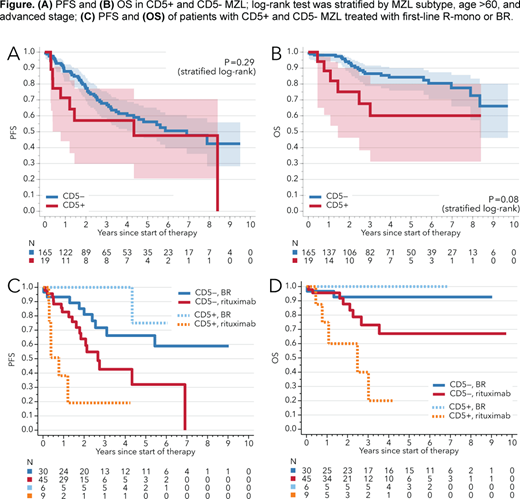
The most common first-line treatments were R-mono (29%), radiation therapy (23%), BR (20%), and surgery (15%). CD5 expression was not prognostic for PFS (stratified log-rank, P=.29, Fig. A) or OS (P=.08; Fig. B) in the entire cohort, or within the subgroup of NMZL/SMZL only (P=.46 for PFS and P=.31 for OS). However, outcomes differed according to CD5+/- status between patients treated with first-line R-mono or BR. ORR to R-mono was significantly lower for CD5+ than CD5- MZL (22% vs. 78%, P=.003), whereas ORR to BR did not differ (100% and 93%, respectively, P=.72). Similarly, PFS after R-mono was significantly worse for CD5+ than CD5- MZL (P=.036; Fig. C), while it did not significantly differ after BR (P=.64; P for interaction between treatments=.030). CD5 expression was also associated with significantly worse OS among patients receiving R-mono (P=.047) but not among those receiving BR (P=.56; Fig. D). Results were similar in the subgroup of SMZL/NMZL cases.
Conclusions. To our knowledge, this is the first study examining CD5 expression as a prognostic and predictive biomarker for outcomes of R-based immunochemotherapy in MZL. CD5+ MZL was characterized by disseminated presentation with universal peripheral blood involvement, but after adjustment for other factors, CD5 expression was not independently prognostic. However, we observed worse response rates, PFS, and OS for CD5+ MZL treated with first-line R monotherapy, but not among those treated with BR, suggesting that the BR combination might be preferable in this subgroup.
Olszewski:Spectrum Pharmaceuticals: Research Funding; Genentech, Inc.: Research Funding; Adaptive Biotechnologies: Research Funding; TG Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.